Health Desk
Sandeep Dhand Ludhiana
Journalist & Research Analysist
Introduction
Leptospirosis is a bacterial infection caused by a type of bacteria called Leptospira. This zoonotic disease, which means it can spread from animals to humans, affects millions of people around the world, especially in tropical and subtropical climates. Leptospirosis is transmitted through direct or indirect contact with the urine of infected animals, such as rodents, farm animals, or pets. This disease can cause a range of symptoms, and in some cases, it can lead to severe complications like liver failure, kidney damage, or even death. In this article, we will explore leptospirosis in detail, including its causes, symptoms, risk factors, diagnosis, treatment, and prevention strategies.
Causes and Transmission
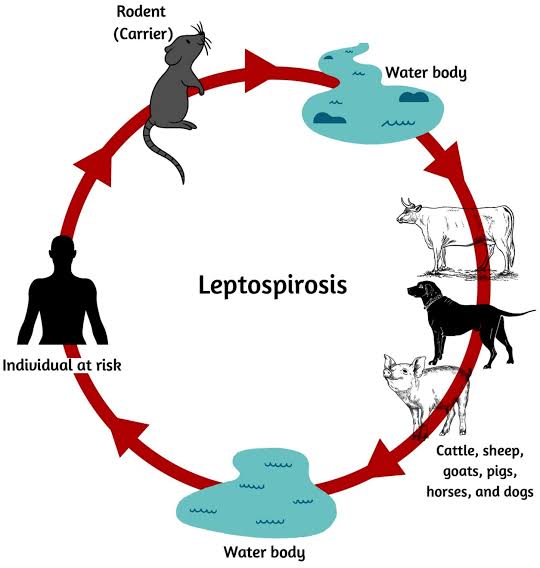
Leptospirosis is caused by the spiral-shaped bacteria known as Leptospira. It primarily affects wild and domestic animals, with rodents, particularly rats, being the main carriers of the bacteria. Other animals such as cattle, pigs, dogs, and horses can also harbor the bacteria. These animals shed the bacteria in their urine, which then contaminates soil and water bodies.
Humans become infected with leptospirosis through contact with contaminated water, soil, or food. The bacteria can enter the body through cuts or abrasions on the skin, as well as through mucous membranes in the eyes, nose, or mouth. Swimming in or drinking contaminated water can also result in infection. The disease is often associated with occupations or activities that involve close contact with animals or environments where the bacteria thrive, such as farming, sewage work, or adventure sports like kayaking and rafting.
Symptoms of Leptospirosis
The symptoms of leptospirosis can vary widely, ranging from mild, flu-like symptoms to severe illness. The incubation period for leptospirosis is usually between 5 to 14 days, but it can range from 2 to 30 days. The symptoms are generally categorized into two phases:
- Initial Phase (Acute Phase):
This phase typically lasts for about a week and presents with symptoms similar to flu. The symptoms may include:
Sudden high fever
Headache
Chills
Muscle aches, particularly in the calves and lower back
Vomiting
Red eyes (conjunctival suffusion)
Rash
Abdominal pain
Some individuals may recover after this phase without further complications, while others may progress to the second, more severe phase.
- Second Phase (Immune Phase or Weil’s Disease):
In severe cases, leptospirosis progresses to what is known as Weil’s disease, which can lead to life-threatening complications. Symptoms of this phase may include:
Jaundice (yellowing of the skin and eyes)
Kidney failure
Liver damage
Difficulty breathing
Irregular heartbeat
Meningitis (inflammation of the membranes around the brain and spinal cord)
Bleeding (such as nosebleeds or bleeding into the skin)
The severity of symptoms can vary, and while some people may only experience mild illness, others can suffer from severe, multi-organ failure requiring intensive medical care.
Risk Factors
Leptospirosis can affect anyone who comes into contact with the bacteria, but certain factors increase the risk of infection. These include:
- Occupational Exposure: People working in agriculture, especially rice and sugarcane farming, are at higher risk due to regular contact with contaminated soil and water. Veterinarians, sewage workers, dairy farmers, and those in animal slaughterhouses are also at increased risk.
- Outdoor Activities: People who engage in outdoor activities, such as camping, swimming, kayaking, and rafting in freshwater bodies, are more likely to be exposed to contaminated water.
- Environmental Factors: Leptospirosis is more common in areas with high rainfall, as flooding can increase the spread of the bacteria. Tropical and subtropical regions are particularly affected due to favorable environmental conditions for the bacteria.
- Household Pets: Pet owners, particularly those with dogs, can be at risk if their pets become infected. Dogs can get leptospirosis from contact with infected animals or contaminated water, and they can pass the bacteria to humans.
Diagnosis
Diagnosing leptospirosis can be challenging due to its nonspecific symptoms, which can resemble many other diseases such as influenza, dengue, or malaria. Physicians often rely on a combination of patient history, physical examination, and laboratory tests to diagnose leptospirosis.
Blood and Urine Tests: Blood and urine samples can be tested for the presence of Leptospira bacteria. Early in the illness, the bacteria can be detected in the blood, while later in the disease, they may be present in the urine.
Serologic Tests: These tests detect antibodies produced in response to the Leptospira bacteria. The Microscopic Agglutination Test (MAT) is the most commonly used serologic test for confirming leptospirosis.
Molecular Tests: Polymerase chain reaction (PCR) is a molecular technique used to detect the bacterial DNA in blood, urine, or cerebrospinal fluid. It is a rapid and highly sensitive method for diagnosing leptospirosis, especially in the early stages of the disease.
Treatment
The treatment for leptospirosis largely depends on the severity of the infection. Early diagnosis and appropriate treatment can significantly reduce the risk of complications. The main treatment options include:
- Antibiotics: Antibiotics are the cornerstone of leptospirosis treatment. Commonly prescribed antibiotics include doxycycline and penicillin. For mild cases, oral antibiotics are sufficient, while severe cases may require intravenous antibiotics.
- Hospitalization: Severe cases of leptospirosis, such as those with liver or kidney involvement, may require hospitalization. Supportive care, including intravenous fluids, dialysis, and respiratory support, may be necessary for patients with complications like organ failure.
- Pain and Fever Management: Pain relievers and antipyretics (fever reducers) are often used to manage symptoms like muscle aches and fever.
Prevention
Preventing leptospirosis involves taking measures to reduce the risk of exposure to contaminated water and soil. Here are some key preventive strategies:
- Avoid Contact with Contaminated Water: Refrain from swimming or wading in water that may be contaminated with animal urine, especially in areas where leptospirosis is common. Wear protective clothing, such as boots and gloves, if you need to work in such environments.
- Control Rodents: Since rodents are major carriers of Leptospira, it is important to take measures to control rodent populations, especially in and around your home. Seal entry points and keep food in rodent-proof containers.
- Personal Hygiene: Wash your hands thoroughly after handling animals or coming into contact with potentially contaminated soil or water. Always cover cuts and abrasions with waterproof dressings to reduce the risk of bacteria entering the skin.
- Vaccination of Animals: Vaccinating pets, such as dogs, against leptospirosis can reduce the risk of transmission to humans. In some countries, livestock are also vaccinated to prevent the spread of the bacteria.
- Chemoprophylaxis: In high-risk situations, such as during outbreaks or when engaging in water-related activities, taking doxycycline as a preventive measure may be recommended. This should only be done under medical guidance.
Conclusion
Leptospirosis is a potentially serious bacterial infection that can cause significant health issues if not properly managed. While the disease is most common in tropical and subtropical regions, it can occur anywhere that individuals come into contact with contaminated water or animals. Recognizing the symptoms and seeking timely medical treatment are essential for reducing the severity of the disease and preventing complications. Preventive measures such as avoiding contact with contaminated water, practicing good hygiene, and controlling rodent populations can effectively reduce the risk of leptospirosis. With greater awareness and proper precautions, the burden of leptospirosis can be minimized, ensuring better health outcomes for individuals at risk.
