Health Desk
Sandeep Dhand Ludhiana
Journalist & Research Analysist
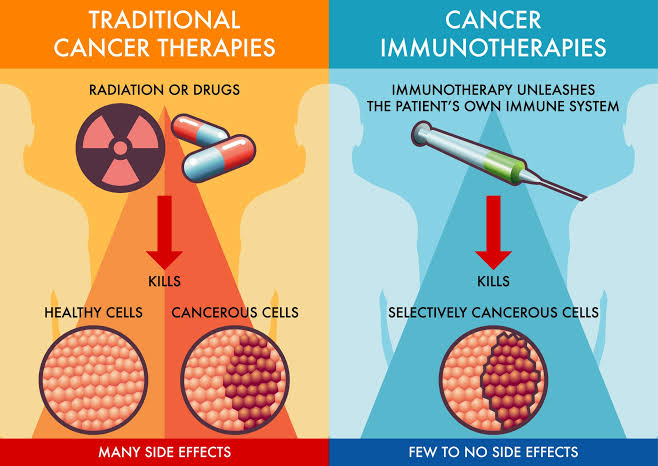
Immunotherapy, also known as biological therapy, is a breakthrough in medical science that uses the body’s immune system to fight diseases, primarily cancer. Unlike traditional treatments like chemotherapy or radiation therapy, which target the disease directly, immunotherapy aims to enhance or manipulate the immune system’s natural capacity to recognize and destroy harmful cells. This therapeutic approach is changing the landscape of cancer treatment, providing new hope for patients with conditions once considered untreatable.
What is Immunotherapy?
The human immune system is a complex network of cells, tissues, and organs that works to defend the body against harmful invaders, such as viruses, bacteria, and even cancer cells. Immunotherapy leverages this natural defense mechanism to attack diseased cells while minimizing damage to healthy tissues.
Cancer cells are particularly challenging for the immune system to detect and destroy because they can disguise themselves as normal cells or suppress the immune system’s response. Immunotherapy seeks to overcome these challenges by enhancing the immune system’s ability to recognize and target cancer cells more effectively.
Types of Immunotherapy
There are several types of immunotherapy, each with its unique mechanism of action:
- Checkpoint Inhibitors: Checkpoint inhibitors are drugs that help the immune system recognize and attack cancer cells by blocking proteins that would otherwise suppress the immune response. Cancer cells often produce these proteins to “hide” from the immune system. By inhibiting these checkpoints, the immune system is free to target the cancer cells. Common checkpoint inhibitors include drugs like pembrolizumab (Keytruda) and nivolumab (Opdivo), which have shown promising results in treating cancers such as melanoma, lung cancer, and more.
- CAR T-cell Therapy: Chimeric Antigen Receptor (CAR) T-cell therapy is an innovative treatment that involves modifying a patient’s T-cells (a type of immune cell) to enhance their ability to attack cancer cells. T-cells are extracted from the patient’s blood and genetically engineered in the lab to produce receptors on their surface that help them target specific cancer cells. These modified T-cells are then infused back into the patient, where they multiply and attack the cancer. CAR T-cell therapy has been particularly effective in treating certain types of blood cancers, such as acute lymphoblastic leukemia and diffuse large B-cell lymphoma.
- Monoclonal Antibodies: Monoclonal antibodies are laboratory-made proteins that can target specific antigens on the surface of cancer cells. These antibodies can work by directly attacking the cancer cells or by marking them so the immune system can find and destroy them. Monoclonal antibodies can also carry other drugs or radioactive substances directly to cancer cells, enhancing their effectiveness. Examples include trastuzumab (Herceptin) for breast cancer and rituximab (Rituxan) for non-Hodgkin lymphoma.
- Cancer Vaccines: Cancer vaccines are designed to stimulate the immune system to prevent or treat cancer. Unlike traditional vaccines that prevent infectious diseases, cancer vaccines can either be preventive (like the HPV vaccine, which reduces the risk of cervical cancer) or therapeutic (designed to boost the body’s response to an existing cancer). Therapeutic cancer vaccines, such as the sipuleucel-T (Provenge) for prostate cancer, are being developed to target cancer cells specifically and improve survival outcomes.
- Cytokine Therapy: Cytokines are proteins that play an essential role in modulating the immune system. In cytokine therapy, synthetic versions of these proteins, such as interleukins and interferons, are used to enhance the immune response against cancer. For instance, interleukin-2 (IL-2) can stimulate the growth of immune cells that are capable of targeting cancer.

How Immunotherapy Works
To understand how immunotherapy works, it’s essential to understand the concept of immune surveillance. The immune system constantly monitors the body for abnormal or harmful cells, eliminating them before they become problematic. However, cancer cells can develop mechanisms to avoid detection by the immune system or to suppress immune activity.
Immunotherapy counteracts these mechanisms by:
Boosting Immune Response: Immunotherapy can enhance the activity of the immune system so that it can effectively identify and destroy cancer cells. For instance, drugs like interleukin-2 can activate immune cells to kill cancer cells.
Overcoming Immune Suppression: Cancer cells often produce substances that suppress the immune system, allowing them to grow unchecked. Checkpoint inhibitors work by blocking these suppressive signals, allowing the immune system to mount a stronger attack.
Targeting Specific Antigens: Monoclonal antibodies are designed to bind to specific proteins found on cancer cells, marking them for destruction by immune cells.
Benefits of Immunotherapy
- Specific Targeting: One of the most significant advantages of immunotherapy over conventional cancer treatments is its specificity. While chemotherapy and radiation often damage both cancerous and healthy cells, immunotherapy targets only the cancer cells, leading to fewer side effects.
- Long-term Protection: Immunotherapy has the potential to provide long-term protection against cancer by training the immune system to remember and recognize cancer cells in the future, thereby reducing the risk of recurrence.
- Effective Against Various Cancers: Immunotherapy has shown success in treating different types of cancers, including those that are resistant to other treatments. For example, melanoma, which was once difficult to treat in its advanced stages, has seen improved survival rates thanks to immunotherapy.

Challenges and Side Effects
While immunotherapy represents a significant advancement in cancer treatment, it is not without challenges and limitations:
- Not Effective for All Patients: Immunotherapy does not work for everyone. The effectiveness can vary depending on the type of cancer, the stage at which it is diagnosed, and the patient’s unique immune response. Research is ongoing to understand why some patients respond well to immunotherapy, while others do not.
- Side Effects: Immunotherapy can cause side effects because it stimulates the immune system, which can sometimes lead to the immune system attacking healthy cells. Common side effects include fatigue, skin reactions, fever, and, in some cases, more severe immune-related adverse events that affect organs like the lungs, liver, or intestines.
- High Costs: Immunotherapy treatments can be expensive, making access a barrier for many patients. The costs associated with developing, manufacturing, and administering these advanced therapies contribute to their high price, limiting widespread availability.
Future of Immunotherapy
Immunotherapy is still a relatively new field, and research is rapidly evolving. Scientists are working on finding biomarkers that can predict a patient’s response to immunotherapy, personalizing treatments to increase their effectiveness. Combining immunotherapy with other forms of treatment, such as chemotherapy or targeted therapy, is also being explored to improve patient outcomes.
Furthermore, ongoing advancements in CAR T-cell therapy, cancer vaccines, and monoclonal antibodies are expanding the scope of cancers that can be treated using immunotherapy. These innovations have the potential to transform cancer from a life-threatening disease into a manageable condition, improving survival rates and quality of life for many patients.
Conclusion
Immunotherapy represents a revolutionary approach in the fight against cancer, offering a new level of hope for patients who previously had limited treatment options. By harnessing the power of the immune system, immunotherapy targets cancer in a way that is specific, effective, and less damaging to healthy cells. Though challenges remain in making these treatments more universally accessible and effective for all patients, ongoing research and innovation in immunotherapy continue to push the boundaries of what is possible in cancer care. As we advance our understanding of the immune system and its capabilities, immunotherapy is poised to become an integral part of modern medicine, changing how we perceive and treat cancer.